Melanoma and Skin Cancer Awareness Month

by Laura Monaghan, PA-C
May brings warm weather, prom season, and spending time poolside. In the world of dermatology, May also brings Melanoma and Skin Cancer Awareness Month. Skin cancer is the most common cancer in the United States, and melanoma is the second most common form of cancer in females ages 15-29. Melanoma rates have doubled from 1982 to 2011, and on average one American dies of melanoma every hour. So, what exactly is melanoma? And what can you do about it?
What is Melanoma?
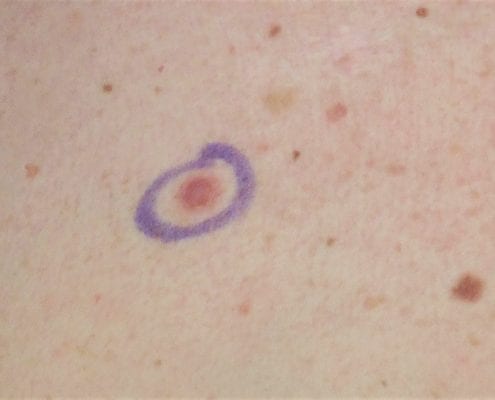
Melanoma is a form of cancer that originates in melanocytes, the cells that produce skin pigment. Damage to the cell’s DNA allows the melanocytes to grow uncontrollably. This can present as a changed mole, a new dark spot, or even a pink nodule on the skin. There are multiple factors that can increase your risk of developing melanoma, which includes:
- Family history of melanoma
- Tanning bed use
- Sun exposure
- Increased age
- More than 50 moles, large moles, or atypical moles
- Fair skin and light hair/eye color
- Personal history of melanoma or other skin cancer
- Personal history of other cancers
Base Tan
Despite the popular idea of getting a “base tan” to kickstart the summer, there is no such thing as a safe tan. In fact, according to the Skin Cancer Foundation, just one indoor tanning session before age 35 increases the risk of developing melanoma by 75%. The risk increases with every subsequent use.
How to prevent skin cancer
Prevention and early detection are key goals of melanoma care. This includes avoiding the sun during the highest UV index hours (10AM-4PM) and wearing SPF 30+ sunscreen, sun-protective clothing and hats, and sunglasses. Routine full-body skin exams with your dermatologist and monitoring your skin at home are also recommended for early detection. Click here to learn what to signs to look for during your skin exam.
Check out this video of Dr. Skelsey and one of her melanoma patients.
Sources:
American Academy of Dermatology. (2018-2020). Key Messages.
Chien, A., & Jacobe, H. (2022, July). Tanning & Your Skin. The Skin Cancer Foundation. Retrieved May 7, 2023, from https://www.skincancer.org/risk-factors/tanning/#:~:text=Indoor%20Tanning%20Dangers&text=increased%20risk%20of%20developing%20life,a%20sign%20of%20skin%20damage.
Indoor tanning. American Academy of Dermatology. (2021, June 21). Retrieved from https://www.aad.org/media/stats-indoor-tanning#:~:text=Using%20tanning%20beds%20before%20age,risk%20increases%20with%20each%20use.&text=Women%20younger%20than%2030%20are,melanoma%20if%20they%20tan%20indoors